| |
|
| Overview / Aminoglycosides / Noise Trauma / Excitotoxicity / Presbycusis / Tinnitus | |
| Pictures : R. Pujol |
 R.Pujol |
|
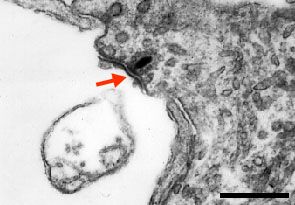
| Immediately after perilymphatic
perfusion with glutamate or its agonists such as AMPA or kainate (ref.c1,
c3), all afferent dendrites below the IHC are swollen, their membranes
are ruptured and their cytoplasmic content is lost (left). At higher
magnification (right), a remnant of the postsynaptic membrane (red arrow)
faces a presynaptic body. The IHC is disconnected from the auditory
nerve and cochlear potentials
are lost. The same type of damage occurs immediately after acoustic
trauma (ref.
c5) or ischaemia (ref.c1,
c3) but it can be blocked by an AMPA antagonist such as DNQX. A
protective effect of dopamine, a lateral efferent neurotransmitter,
is also observed. scale bar: 10 µm (Left); 0,3 µm (right). |
|
|
|
||
|
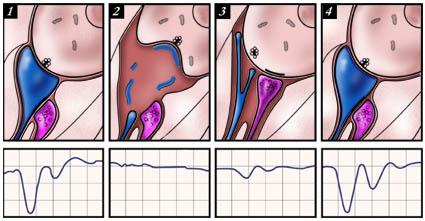
1) Normal
synaptic complex below an IHC:
a presynaptic body in the IHC faces an afferent dendrite (blue), which
itself is contacted by a lateral efferent vesiculated ending (pink).
The cochlear action potential is normal. In man, this mechanism is probably the
basis for recovery after sudden deafness caused by ischaemia or noise
trauma. |
 JL. Puel |
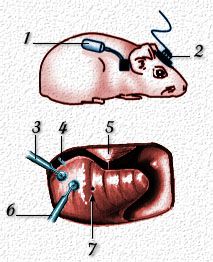
1- osmotic
minipump (Azlet Corp) which delivers a drug (eg agonist, antagonist,
antisense molecule) over 3,5,7, or 15 days. After placing the catheter
in a tiny hole in the scala tympani (3), the pump is inserted under
the dorsal skin; 2- recording plug to monitor cochlear potentials: the plug is connected to the round window electrode (4); 5- eardrum; 6- micropipette which delivers a single shot of drug (for instance, AMPA to induce excitotoxicity) or chronic dose if connected to minipump; 7- hole (in scala vestibuli) for perfusion outlet (for acute pharmacology). |
| This protocol
of intracochlear perfusion is used in animals (guinea pigs or rats)
to explore the molecular pharmacology of the first auditory synapse
in the cochlea. Currently this protocol is being used to check the effect of molecules in speeding up the repair process, protecting the neurone, or stopping an increased firing of the fibre (tinnitus). In humans, whilst intracochlear pharmacology cannot be envisaged, a substitutive trans-tympanic protocol is going to be tested. In this way in the near future a specific and local pharmacology for the cochlea may be successfully developed. |
|
 JL.
Puel et al.
JL.
Puel et al.