| |
|
| Overview / Aminoglycosides / Noise Trauma / Excitotoxicity / Presbycusis / Tinnitus | |
| Pictures : M. Lenoir |
| Tinnitus |
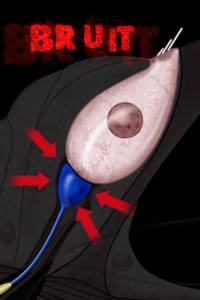
Together with hearing loss, hair cell and neuronal pathologies may also account for the origin of tinnitus (an auditory perception in the absence of any sound stimulation of the cochlea). Clinicians classify a variety of types of tinnitus, of which some have an extra-cochlear (vascular or muscular) origin. However, the vast majority of tinnitus manifests as ringing noises of mid- or high frequency and most of these types of tinnitus probably have a cochlear origin. With the passage of time, higher levels of the auditory pathway may be involved, and the perception of tinnitus may not depend on the cochlear pathology any longer. To date, two main hypotheseses concerning the cochlear trigger of tinnitus have been proposed. The first one involves spontaneous OHC electromotility, the second one the glutamatergic synapse between IHC and auditory nerve. While the former is not really supported by experimental data, the later hypothesis is becoming stronger. |
| Tinnitus and OHCs |
| It has been hypothesised that spontaneous OHC electromotility may cause an activation of IHCs and auditory nerve fibres. A defect in the modulation by the medial efferent system has also been postulated. However, no direct evidence has been provided. Moreover, only very rarely have spontaneous oto-acoustic emissions been correlated with an objective ringing in the ear. |
| Tinnitus and synapses | ||
| This hypothesis is getting more and more support from recent experimental findings; it tends to consider tinnitus as sort of "epileptic" firing in the auditory nerve. NMDA glutamate receptors, which are overexpressed after excitotoxic injury, especially after noise trauma or ischaemia, may well be the trigger of an increased spontaneous firing in the auditory nerve. In turn, the auditory area in the brain would decode this locally increased firing as a sound. It is interesting to note that salicylate, well known to precipitate tinnitus, causes just such an increased spontaneous firing rate in the auditory nerve. Post-traumatic tinnitus is perceived at a frequency just where the audiogram strarts to deteriorate. This fits with the idea that remaining nerve endings have been damaged enough to overexpress NMDA receptors, thus increasing their spontaneous firing. | ||
 |
 |
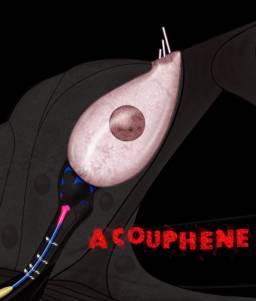 |
| Normal synapse | (BRUIT
= NOISE / ACOUPHENE = TINNITUS) Traumatic noise = disruption of synapse = tinnitus click to see animation (4MO) |
|
After the last experiments in JL Puel's group have been done to assess the validity of this hypothesis, some local treatment of tinnitus may well be proposed, aiming specifically to cure the IHC-auditory nerve synapse dysregulation. Other possibilities involving
the IHC-auditory nerve synapse are being studied, for example
for a possible defect in lateral efferent tonic inhibition. |
||
